GMHC has dramatically expanded its mental health and substance use services since Chet Balram, Managing Director for Mental Health and Substance Use, and his colleague Keila Morales, Managing Director of Clinic Operations, joined the agency three years ago with that mandate.
“Our vision is to ensure that everyone that walks through GMHC’s door is able to access mental health and substance use services,” says Balram.
They are getting closer to that goal. GMHC now provides mental health services to over 200 clients through its Article 31 clinic and federally funded Ryan White HIV/AIDS programs. By contrast, the Article 31 clinic had just 20 clients, who were not actively engaged in services, when Balram and Morales joined GMHC in 2021.
“The Article 31 clinic is thriving. We’re at capacity and, as we continue to grow, we see the need for mental health services in our community,” Balram says. The Article 31 clinic serves both HIV positive and negative clients through a fee-for-service model. The Ryan White-funded mental health services are for people living with HIV and are free of charge.
Last year, the Mental Health and Substance Use Department delivered 4,567 counseling sessions – an extraordinary 45% increase from the 3,139 delivered in 2022, the first full year of operations under Balram and Morales. What’s more, the program was awarded a grant from SAMHSA (Substance Abuse and Mental Health Services Administration) to provide harm-reduction care to anyone over age 18 seeking help with substance use – regardless of HIV status.
“People are coming to us because of the client-centered, trauma-informed culture we’ve created in the mental health department,” says Balram, noting that referrals come from within the agency and partners such as Mt. Sinai, Callen-Lorde, and the Alliance for Positive Change.
“Some of our clients have experienced trauma and violence. A lot of our LGBTQ+ and transgender clients continue to experience abuse and violence related to their identity, as well as their HIV status,” he says.
GMHC takes a nonjudgmental, stigma-free, and culturally competent approach to mental health care, Balram adds. “We work with our clients on their goals – not what we think their goals should be. We are meeting them where they’re at.”
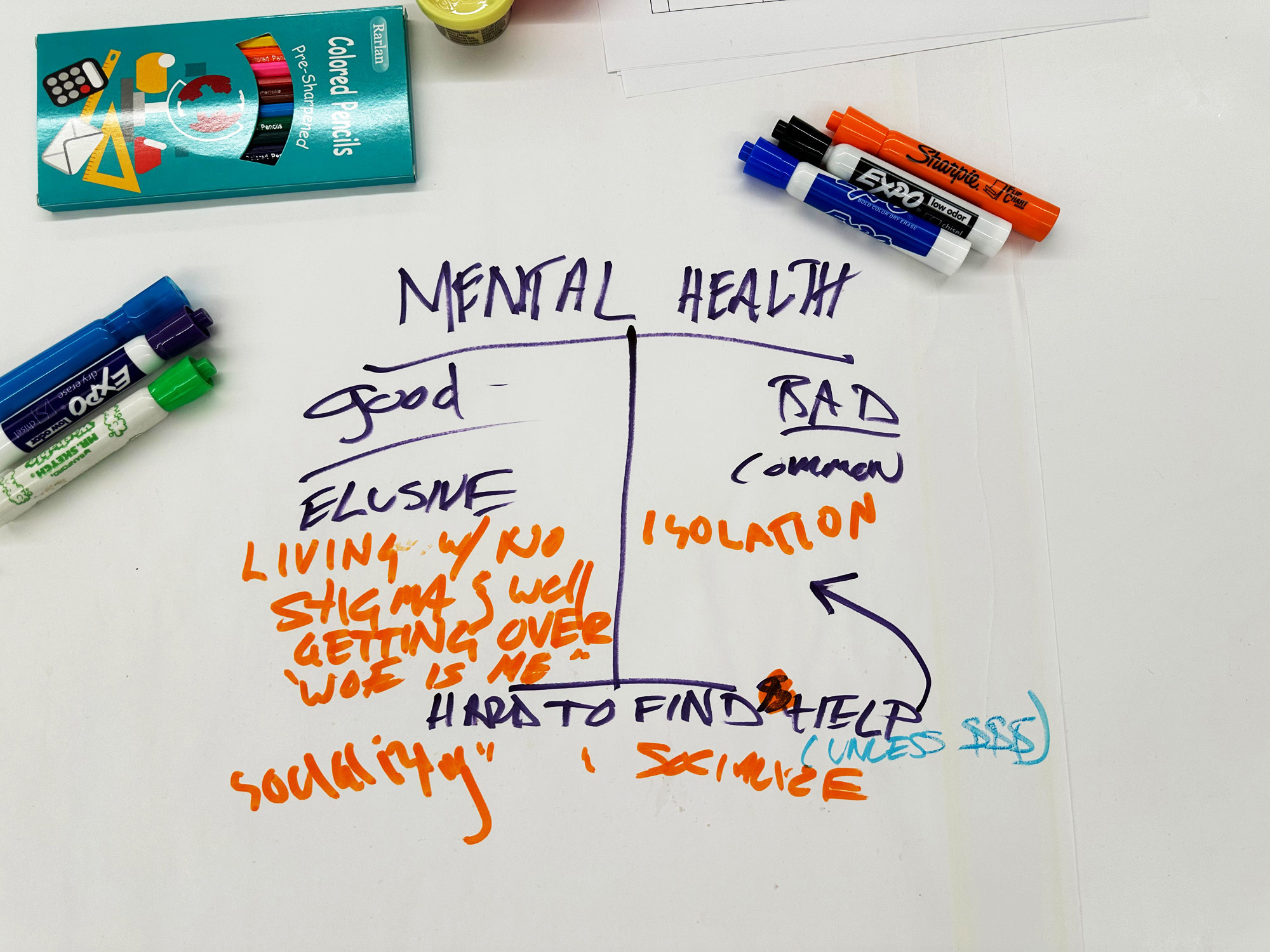
Clients are experiencing other life stressors as well. For instance, many are over age 50 so they’re negotiating aging with HIV. “Issues that come up are isolation, relationships, and living with HIV,” Balram says. “What support do they need to live in a healthier way in as they age?”
GMHC’s mental health services include individual and group counseling, medication management, and opioid overdose prevention training. The mental health team works closely with their harm-reduction colleagues, since these are often co-occurring disorders. “Clients may be using substances to numb the mental health symptoms, so we want to make sure they receive appropriate care,” Balram says.
What’s more, the mental health team offers support groups that are open to all GMHC clients, ranging from “Coping and Connecting with Life Challenges” to “Sex, Love & Intimacy” to groups for long-term HIV survivors and crystal meth users.
Supportive Circle
Many clients’ mental health and substance use issues are coupled with basic unmet needs, such as adequate nutrition and stable housing. “As part of our client assessment, we find out their other needs and how we can support them,” Morales says.
The mental health team often connects clients to additional GMHC programs. “We work together with a client’s case managers in other departments to get them to where they want to be,” Morales explains.
For instance, a client receiving supportive housing services could start missing appointments with their mental health counselor. As a hypothetical for client confidentiality, the client’s housing case manager could learn on an at-home health visit that they are grappling with substance use. With the client’s permission, the case manager would share that with their counselor, and the two would schedule ongoing case conferences to best support the client.
“That collaboration can help a client who might otherwise drop out of counseling,” Morales says.
Balram and Morales have built a team that forms a supportive circle. Through group supervision with Balram and regular case conferences, mental health counselors discuss clients’ challenges and track their progress with the team’s psychiatrist, nurse practitioner, and clinical supervisor.
“We are looking at the whole person and making sure the client’s best interests are being addressed,” Balram says.
As part of the wraparound approach, client navigators help clients connect to supportive services outside of the agency. “We follow up and make sure clients can overcome any barriers they may encounter in receiving services,” Morales says.
They’ve expanded the team to 31 total mental health staff, up from seven when they joined GMHC. “Our team is fantastic. Everyone is incredibly supportive of each other – and that’s what we look for when hiring,” Balram says.
Several of the team’s clinical supervisors are now expanding clinical support and training on trauma-informed care to client-facing staff in other departments, starting with the supportive housing, testing and prevention, and workforce development teams. “Collaborative care is really the essence of great care,” Morales says.